Streamline hiring with effortless screening tools
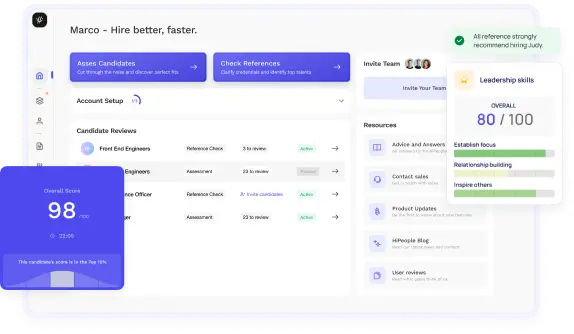
Optimise your hiring process with HiPeople's AI assessments and reference checks.

Have you ever wondered what sets apart exceptional healthcare professionals from the rest? It's not just about technical expertise or medical knowledge—oftentimes, it's the soft skills they possess that make all the difference. In the fast-paced and emotionally charged environment of healthcare, the ability to communicate effectively, empathize with patients, collaborate seamlessly with colleagues, and adapt to ever-changing circumstances is paramount. These soft skills, also known as interpersonal skills, are not only essential for delivering high-quality patient care but also for fostering a positive work environment and building trust with patients and their families.
In this guide, we'll explore the top soft skills that healthcare professionals need to succeed, why they matter, and how employers can assess candidates for these critical qualities. Whether you're a healthcare provider looking to enhance your skillset or an employer seeking to build a strong healthcare team, this guide will provide valuable insights to help you navigate the dynamic world of healthcare with confidence and compassion.
Soft skills, often referred to as interpersonal skills or people skills, are non-technical skills that relate to how individuals interact with others, communicate, and navigate social situations. Unlike hard skills, which are specific to a particular job or industry and can be taught and measured, soft skills are more subjective and encompass traits such as communication, emotional intelligence, teamwork, and adaptability.
Soft skills are inherent to an individual's personality and character, influencing how they approach tasks, handle challenges, and collaborate with others. While hard skills are essential for performing technical aspects of a job, soft skills are critical for building relationships, fostering teamwork, and delivering quality service in various professional settings, including healthcare.
Soft skills are integral to the delivery of high-quality patient care and the effectiveness of healthcare teams. In the fast-paced and often emotionally charged environment of healthcare, professionals must possess strong interpersonal skills and emotional intelligence to navigate complex interactions and provide patient-centered care. Some key reasons why soft skills are crucial in healthcare include:
Soft skills are not only essential for individual healthcare professionals but also for the overall functioning of healthcare organizations. By prioritizing the development and assessment of soft skills in their workforce, healthcare organizations can enhance patient satisfaction, improve clinical outcomes, and create a positive and supportive work environment for their employees.
Effective communication is the cornerstone of successful interactions in the healthcare setting. It involves more than just speaking or listening—it's about understanding, empathy, and clarity.
Active listening isn't just about hearing words; it's about understanding the underlying emotions and concerns of patients and colleagues. In healthcare, active listening is crucial for building trust, gathering accurate information, and addressing patient needs effectively. Healthcare professionals practice active listening by giving their full attention, maintaining eye contact, and paraphrasing to confirm understanding.
Clear and concise verbal communication is vital in conveying information accurately and avoiding misunderstandings. Healthcare professionals must tailor their language to suit the comprehension levels of their audience, whether they're speaking to patients, colleagues, or family members. Avoiding medical jargon, using simple language, and providing explanations in understandable terms are key aspects of effective verbal communication in healthcare.
Non-verbal cues such as facial expressions, body language, and gestures can convey emotions and messages that words alone may not express. In healthcare, understanding and interpreting non-verbal communication can help professionals gauge patient comfort, assess pain levels, and detect anxiety or distress. Being mindful of one's own non-verbal cues and observing those of others are essential skills for effective communication in healthcare settings.
Empathy and compassion lie at the heart of patient-centered care. Empathy involves understanding and sharing the feelings of others, while compassion entails expressing kindness and concern for their well-being. Healthcare professionals demonstrate empathy and compassion by listening actively, validating patients' experiences, and showing genuine care and support. These qualities not only enhance patient satisfaction but also contribute to better clinical outcomes and overall quality of care.
In the fast-paced environment of healthcare, collaboration and teamwork are essential for providing comprehensive care and ensuring positive patient outcomes. Healthcare professionals must work together seamlessly, leveraging each other's expertise and perspectives to deliver high-quality care.
Interdisciplinary collaboration involves healthcare professionals from different specialties and disciplines coming together to address the complex needs of patients. Each team member brings unique knowledge and skills to the table, and effective communication and mutual respect are essential for successful collaboration. By working collaboratively, healthcare teams can develop comprehensive care plans, coordinate services, and optimize patient outcomes.
Conflicts are inevitable in any team environment, but how they are managed can make a significant difference in team dynamics and patient care. Healthcare professionals must be adept at resolving conflicts constructively, addressing underlying issues, and finding mutually acceptable solutions. Open communication, active listening, and a focus on shared goals can help teams navigate conflicts effectively and maintain a positive working environment.
Healthcare is a dynamic field with ever-changing demands and challenges. Healthcare professionals must be flexible and adaptable, ready to adjust their approaches in response to evolving patient needs, new technologies, and emerging trends. Flexibility involves being open to new ideas, willing to learn from others, and embracing change as an opportunity for growth. By cultivating flexibility and adaptability, healthcare teams can thrive in the face of uncertainty and deliver innovative solutions to complex problems.
Supporting colleagues is not just about lending a helping hand; it's about fostering a culture of collaboration, trust, and mutual respect within the healthcare team. Healthcare professionals can support their colleagues by offering assistance, sharing knowledge and expertise, and providing emotional support during challenging times. By nurturing a supportive work environment, healthcare teams can boost morale, reduce burnout, and ultimately deliver better care to their patients.
Emotional intelligence (EI) plays a crucial role in the healthcare profession, impacting how professionals interact with patients, colleagues, and themselves. It comprises several key components that contribute to effective communication, relationship building, and decision-making.
Self-awareness involves understanding one's own emotions, strengths, weaknesses, and how they affect others. In healthcare, self-awareness enables professionals to recognize their biases, triggers, and limitations, allowing them to regulate their behaviors and responses appropriately. Through self-reflection, feedback from peers, and ongoing personal development, healthcare professionals can enhance their self-awareness and improve their interactions with others.
Self-regulation refers to the ability to manage and control one's emotions, impulses, and reactions in different situations. Healthcare professionals often encounter high-stress environments where emotions can run high, making self-regulation essential for maintaining professionalism and providing quality care. Techniques such as deep breathing, mindfulness, and cognitive reframing can help professionals manage stress, remain calm under pressure, and make sound decisions in challenging circumstances.
Social awareness involves understanding the emotions, needs, and perspectives of others, including patients, colleagues, and the broader community. In healthcare, social awareness enables professionals to empathize with patients, anticipate their needs, and tailor care plans to meet their preferences effectively. Active listening, empathy, and cultural competence are essential skills for developing social awareness and building rapport with diverse patient populations.
Relationship management encompasses building and maintaining positive relationships with patients, colleagues, and other stakeholders in the healthcare setting. Strong interpersonal skills, effective communication, and conflict resolution abilities are essential for fostering trust, collaboration, and teamwork. Healthcare professionals who excel in relationship management can navigate complex interpersonal dynamics, resolve conflicts constructively, and promote a supportive work environment conducive to patient-centered care.
Healthcare professionals encounter a myriad of challenges and uncertainties daily, requiring them to think critically and develop innovative solutions to improve patient outcomes and enhance organizational efficiency.
Analytical skills involve gathering, interpreting, and evaluating information to identify patterns, trends, and insights that inform decision-making. In healthcare, analytical skills are crucial for diagnosing medical conditions, interpreting test results, and developing evidence-based treatment plans. Healthcare professionals use critical thinking and analytical reasoning to assess risks, anticipate potential complications, and make informed decisions that optimize patient care and safety.
Healthcare environments can be fast-paced and high-pressure, necessitating quick and decisive decision-making. Healthcare professionals must weigh the risks and benefits of different options, considering factors such as patient preferences, clinical evidence, and ethical considerations. Effective decision-making under pressure requires a combination of critical thinking, clinical expertise, and situational awareness. Simulation training, role-playing exercises, and case studies can help professionals develop and hone their decision-making skills in realistic scenarios.
Creativity and innovation are essential for identifying novel approaches to patient care, improving processes, and addressing healthcare challenges. Healthcare professionals who think creatively can develop innovative solutions to complex problems, enhance efficiency, and enhance patient satisfaction. Encouraging a culture of innovation, collaboration, and continuous learning can foster creativity among healthcare teams, leading to the development of new technologies, protocols, and care delivery models that transform healthcare delivery.
Healthcare is a dynamic field characterized by constant change, including advancements in technology, evolving patient demographics, and shifting regulatory requirements. Healthcare professionals must be adaptable, ready to adjust their approaches and embrace new opportunities for improvement. Adaptability involves staying abreast of emerging trends, learning new skills, and being open to change. Healthcare organizations can support adaptability by providing professional development opportunities, fostering a culture of learning, and empowering employees to contribute to organizational change efforts.
Patient-centered care lies at the core of healthcare delivery, emphasizing the importance of tailoring treatment to meet the individual needs, preferences, and values of each patient. It involves fostering a collaborative partnership between healthcare providers and patients to achieve optimal health outcomes.
Understanding patient needs and preferences involves more than just medical diagnosis; it requires healthcare professionals to consider the holistic well-being of patients, including their physical, emotional, and psychosocial needs. By actively listening to patients, engaging in shared decision-making, and respecting their autonomy, healthcare professionals can develop personalized care plans that address individual preferences and improve patient satisfaction.
Cultural competency is essential for providing culturally sensitive care that respects the diverse backgrounds, beliefs, and practices of patients from different cultural, ethnic, and socioeconomic groups. Healthcare professionals who are culturally competent demonstrate awareness of their own cultural biases, seek to understand the cultural perspectives of patients, and adapt their communication and care delivery strategies accordingly. By promoting cultural humility and embracing diversity, healthcare organizations can reduce disparities in care and foster trust with underserved populations.
Respect and dignity are fundamental principles of patient-centered care, ensuring that patients are treated with compassion, empathy, and humanity. Healthcare professionals demonstrate respect by acknowledging the inherent worth and rights of each individual, regardless of their medical condition, socioeconomic status, or background. Upholding patient dignity involves maintaining privacy, preserving autonomy, and involving patients in decision-making processes that affect their care. By prioritizing respect and dignity, healthcare professionals can foster trust, enhance communication, and promote positive patient experiences.
Building trust and rapport is essential for establishing a therapeutic relationship between healthcare providers and patients, which is foundational to effective communication, collaboration, and shared decision-making. Trust is earned through consistent, reliable, and transparent interactions, where patients feel valued, heard, and respected. Healthcare professionals can build trust by demonstrating competence, empathy, and integrity, and by honoring their commitments to patients. By nurturing trusting relationships, healthcare providers can enhance patient satisfaction, adherence to treatment plans, and health outcomes.
Effective time management and organization are essential skills for healthcare professionals to maximize productivity, minimize errors, and deliver quality care in a fast-paced environment.
Prioritizing tasks involves assessing the urgency and importance of various responsibilities and allocating time and resources accordingly. Healthcare professionals must triage patient needs, addressing urgent matters promptly while also managing ongoing tasks and responsibilities. Prioritization helps professionals focus on activities that have the greatest impact on patient care and outcomes, ensuring that critical tasks are completed in a timely manner.
Managing workload efficiently requires balancing patient care responsibilities, administrative tasks, and professional development activities effectively. Healthcare professionals can optimize their workflows by implementing time-saving strategies such as delegation, automation, and batch processing. By streamlining processes and eliminating inefficiencies, professionals can increase productivity, reduce burnout, and improve overall job satisfaction.
Meeting deadlines is crucial for maintaining regulatory compliance, completing documentation accurately, and ensuring timely delivery of care. Healthcare professionals must establish realistic timelines for tasks and commitments, using tools such as calendars, reminders, and to-do lists to stay organized and on track. Effective time management and prioritization enable professionals to meet deadlines consistently, reducing the risk of errors and delays in patient care.
Stress is inherent in the healthcare profession, but effective stress management strategies can help professionals cope and thrive in demanding environments. Healthcare professionals can mitigate stress by practicing self-care, seeking support from colleagues and mentors, and engaging in stress-reducing activities such as exercise, mindfulness, and hobbies. By prioritizing their well-being and implementing stress management techniques, professionals can maintain resilience, avoid burnout, and sustain high levels of performance.
Effective leadership is vital for driving innovation, fostering collaboration, and promoting a culture of excellence within healthcare organizations. Healthcare professionals who possess strong leadership skills can inspire and empower their teams to achieve shared goals and deliver high-quality patient care.
Motivating and inspiring others is a key aspect of leadership in healthcare. Effective leaders cultivate a positive work environment where team members feel valued, engaged, and motivated to perform at their best. They communicate a clear vision, set challenging but achievable goals, and recognize and celebrate the contributions of their team members. By inspiring others through their words and actions, healthcare leaders can foster a culture of excellence and continuous improvement.
Delegating tasks effectively involves assigning responsibilities to team members based on their skills, expertise, and workload capacity. Effective leaders empower their team members to take ownership of their tasks, providing clear instructions, resources, and support as needed. They delegate tasks strategically, balancing workload distribution to maximize efficiency and productivity. By trusting their team members and allowing them to contribute meaningfully, leaders can foster a sense of autonomy and accountability that drives performance and innovation.
Conflict is inevitable in any team environment, but effective leaders can address issues promptly and constructively. Leaders facilitate open communication, encourage active listening, and mediate conflicts to find mutually acceptable solutions. They foster a culture of respect, trust, and collaboration, where team members feel comfortable expressing their concerns and working together to resolve differences. By promoting healthy conflict resolution strategies, leaders can strengthen team dynamics and cultivate a supportive work environment that enhances patient care and outcomes.
Leading by example is perhaps the most powerful form of leadership. Effective leaders embody the values, behaviors, and standards they wish to see in their team members. They demonstrate integrity, professionalism, and compassion in their interactions with patients, colleagues, and stakeholders. By modeling a commitment to excellence, continuous learning, and ethical conduct, leaders inspire trust and confidence in their team members and serve as role models for professional growth and development.
Technology plays an increasingly significant role in healthcare delivery, with innovations ranging from electronic health records to telemedicine platforms transforming the way care is delivered and managed. Healthcare professionals must be adaptable and proficient in leveraging technology to improve patient outcomes and streamline workflows.
Proficiency in using healthcare technology is essential for healthcare professionals to navigate electronic health records, clinical decision support systems, and other digital tools effectively. Professionals must undergo comprehensive training to develop proficiency in using these technologies, ensuring accurate documentation, efficient communication, and safe medication administration.
The rapid pace of technological advancement in healthcare requires professionals to stay abreast of new tools and systems continually. Healthcare organizations must invest in ongoing training and professional development opportunities to equip their staff with the skills and knowledge needed to adapt to evolving technologies. Professionals who demonstrate a willingness to learn and embrace new technologies can enhance their effectiveness, improve patient care, and remain competitive in the healthcare industry.
Troubleshooting skills are crucial for resolving technical issues and system failures that may arise when using healthcare technology. Healthcare professionals must be adept at identifying problems, troubleshooting root causes, and implementing solutions quickly to minimize disruptions to patient care. Training programs should include hands-on practice and simulations to develop troubleshooting skills and enhance confidence in using technology effectively.
Integrating technology into patient care requires healthcare professionals to leverage digital tools and systems to enhance clinical decision-making, patient education, and care coordination. Professionals must be proactive in identifying opportunities to use technology to improve patient outcomes, streamline workflows, and enhance the patient experience. By integrating technology seamlessly into patient care processes, healthcare organizations can optimize efficiency, reduce errors, and deliver more personalized and effective care.
Assessing soft skills in candidates is essential for healthcare employers to identify individuals who possess the interpersonal qualities and emotional intelligence necessary to excel in patient care and teamwork. Various methods can be employed to evaluate candidates' soft skills during the hiring process.
Behavioral interview questions are designed to elicit specific examples of past behaviors and experiences that demonstrate candidates' soft skills in action. These questions focus on how candidates have handled various situations in the past, providing insights into their communication style, problem-solving abilities, and teamwork skills. Examples of behavioral interview questions include:
Scenario-based assessments present candidates with hypothetical situations or case studies relevant to the healthcare environment and ask them to outline how they would respond. These assessments simulate real-world scenarios to gauge candidates' critical thinking, decision-making, and problem-solving abilities. Employers can assess candidates' ability to navigate complex situations, prioritize tasks, and communicate effectively under pressure. Examples of scenario-based assessments include:
Pre-employment assessments are standardized tests or questionnaires designed to measure specific soft skills, such as emotional intelligence, communication, and teamwork. These assessments may include personality assessments, situational judgment tests, or emotional intelligence assessments. By administering pre-employment assessments, employers can obtain quantitative data on candidates' soft skills and compare their results against predetermined benchmarks or criteria.
Reference checks involve contacting previous employers, supervisors, or colleagues to gather feedback on candidates' past performance and soft skills. References can provide valuable insights into candidates' communication style, work ethic, and interpersonal skills. Employers can ask specific questions related to the soft skills required for the role and inquire about candidates' strengths, areas for improvement, and overall suitability for the position.
Simulation exercises immerse candidates in realistic scenarios or tasks that simulate aspects of the job they are applying for. These exercises may involve role-playing interactions with patients or colleagues, navigating virtual patient care scenarios, or participating in team-based simulations. Simulation exercises allow employers to observe candidates' soft skills in action, such as communication, problem-solving, and teamwork, in a controlled environment. Feedback from observers or assessors can provide valuable insights into candidates' performance and areas for development.
Employers may use a combination of these methods to comprehensively assess candidates' soft skills and ensure they are well-suited for the demands of the healthcare profession. By selecting candidates who demonstrate strong interpersonal skills, emotional intelligence, and adaptability, employers can build teams that deliver high-quality patient care and foster a positive work environment.
Mastering soft skills is not just an option but a necessity for healthcare professionals aiming to excel in their careers. These interpersonal qualities, including effective communication, empathy, teamwork, adaptability, and leadership, are the cornerstone of providing patient-centered care and fostering positive relationships within healthcare teams. By prioritizing the development of soft skills, healthcare professionals can enhance patient satisfaction, improve clinical outcomes, and create a supportive work environment where collaboration thrives and innovation flourishes.
As we've explored in this guide, assessing soft skills in candidates is crucial for healthcare employers seeking to build strong and cohesive teams. Through behavioral interview questions, scenario-based assessments, pre-employment assessments, reference checks, and simulation exercises, employers can identify candidates who possess the essential soft skills needed to thrive in the dynamic and demanding healthcare environment. By investing in the recruitment and development of professionals with strong soft skills, healthcare organizations can ensure that they deliver high-quality care that meets the diverse needs of patients and contributes to positive health outcomes for all.